Advances in Paraspinal Thermographic Analysis


Harry Wallace, D.C. Joni Wallace, D.C. and Roy Resh, B.S.
————————————————————————
Abstract
Basic theory and common practice in temperature-based chiropractic assessment procedures and instrumentation are reviewed. Segmental spinal thermoregulatory function is presented as a refining mechanism for hypothalamic core-temperature control. Spinal nerve-cell-body function is suggested as the primary mechanism responsible for the asymmetries and anomalies commonly observed in paraspinal and other thermograms. Paraspinal cutaneous thermal asymmetries and anomalies are shown to be suggestive of various pathophysiological alterations, and in particular, the vertebral subluxation complex (VSC). Scientific hypotheses and experimental data relevant to historical and present diagnostic paraspinal thermography are presented, along with a review of representative instrumentation. The potential impact on chiropractic of these postulations, and of newly available, high-precision, computerized spot-radiometry (spot infrared thermography) is examined.
BACKGROUND
Paraspinal cutaneous thermal anomalies have long been held to be suggestive of vertebral subluxation. A review of analytical theories relating to thermography and its use in chiropractic indicated a need for a more complete understanding of the relationship between thermographic data and spinal health. In this study we completed an in-depth review of literature relating to cutaneous thermography, analyzed the basic theory of commonly used instrumentation and postulated new concepts relating to paraspinal thermoceptive neuronal sympathetic function.
Chiropractic – The Early Leader
Historically, temperature measurement has been the most common objective diagnostic modality in health practice. Thermal measurement devices range from simple mercury-in- glass thermometers for core temperature measurement to highly sophisticated thermographic imagers that provide a "picture" of variations in the heat radiated from the skin. In the 1920's, Chiropractors launched into thermography with the Neurocalometer developed by B. J. Palmer and Dossa Evans. This instrument incorporates dual thermocouple thermometers that are mounted two inches apart. Electrically, the thermocouples are differentially connected and their output drives a strip-chart recorder. When the dual thermocouple is moved along the paraspinal skin, the recorder trace represents a scan of differential temperatures. 1,2 The early chiropractic investigators lacked the advantages of modern computerized equipment and rigorous analytical techniques. They did, however, pioneer in the development of these three physiological postulations upon which most clinical cutaneous thermography is based:
1.The human body is segmented into "dermatomes"; 2.Side-to-side skin temperatures are generally symmetrical unless dysfunction exists; 3.Any anomalous deviation from a gradually increasing paraspinal skin temperature from S2 to C1 may suggest the vertebral subluxation complex (VSC) or remote dysfunction. 1-3 There are far reaching health implications in these postulations because they suggest that paraspinal thermography should provide a "window" into the entire sympathetic nervous system. 4
Theory and Practice in Thermo Graphic Assessment
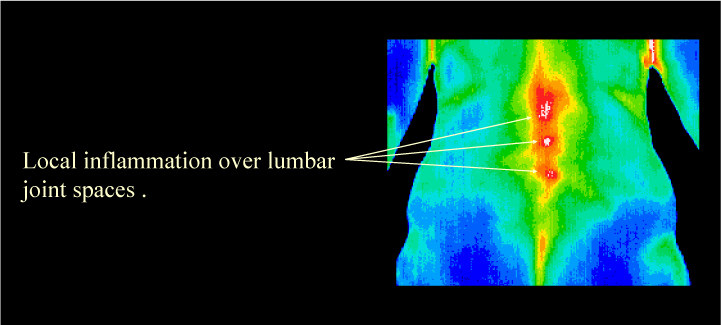
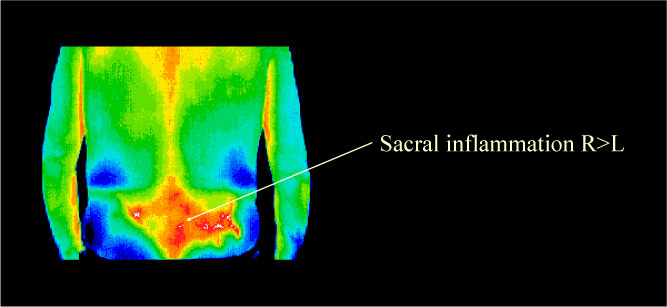
Modern medical theories and clinical findings parallel many of the early thermographic concepts related to chiropractic assessment procedures. As thermal detectors are moved upward from S2 to C1, the NCM and several other chiropractic instruments produce strip chart recorder traces that represent variations in the temperature difference across the spine. Significant temperature anomalies, or "breaks," are said to be suggestive of a VSC. 1-3,5,6 Many investigators have also theorized that any consistent "pattern" in spinal temperature differentials also suggests a VSC. This is the "pattern of interference" theory which proposes that interference with neuronal function at the spinal level creates side-to-side paraspinal thermal anomalies that may persist until the eliciting VSC is corrected. 7 Some practitioners employ analogous single-trace thermography that provides a strip-chart record of the actual temperature along one side of the spine, usually from S2 to C1. Thermal anomalies in these single measurement traces are also said to suggest the location of a VSC.6 Recent thermographic developments also include low-resolution and high-resolution imaging systems and liquid crystal contact sheets. Such "imagers" display grey-scale or color "pictures" representing the thermal pattern of a large skin territory on a video monitor or a flexible sheet. Thermal anomalies in adjacent dermatomes are considered to be suggestive of sympathetic neuronal function. Information relating to sympathetic function in turn helps to localize the VSC and other dysfunctions. 5-8
Medical science has long postulated that definable mechanisms within the sympathetic nervous system give rise to paraspinal cutaneous thermal anomalies. It is generally accepted that various internal and external mechanical, thermal and pain-inducing stimuli elicit sympathetic neuronal response. Thermoregulatory function, which is considered to be primarily sympathetic, is now thought to be centered in the hypothalamus and refined at each spinal-cord segment. 9
This physiological theory, which can account for many normal and abnormal paraspinal skin temperature anomalies, tends to be validated by a wealth of anecdotal and experimental data.10-24 Much of the relevant chiropractic literature emphasizes relief of nerve-pathway interference as the main health benefit from correction of a VSC. On the other hand, modern sympathetic physiological theory, supported by thermographic findings, tends to suggest that relief of noxious sympathetic neuronal function may have more significance. Although it was the early leader, the chiropractic community has waxed and waned in the use of thermographic aids in the assessment of physiology and a VSC. Much of the recent scientific thermographic literature is from the medical community, which seldom considers a VSC as a possible contributor to their findings. The information presented in many of the scientific articles reviewed by the authors, however, strongly support the concept that carefully developed thermographic findings tend to validate chiropractic adjustment as a vital health practice.
Face Validation by Various Practitioners
Thermography, as with many other analytical procedures, has been partially validated by a long history of successful use by experienced practitioners. Glen, Kevin and Brian Stillwagon (D.C.s) are among the most well known advocates of clinical thermography. They assert that chiropractic should concentrate more on correction of the root causes of the abnormal physiology that temperature findings can reveal, and less on anatomical and chemical dysfunction. 25,26 David Ben Eliyahu, D.C., states: "Thermography is a non-invasive, risk-free diagnostic procedure that images cutaneous infrared heat transmission." 27 "A Thermogram is essentially a `heat map' of the dermal contour" according to Timothy Conwell, D.C. Wm. Hobbins, M.D., Director of Thermal Image Analysis, Inc., concludes: "Thermography will offer the practicing Chiropractor an excellent way to objectively document for diagnosis and for demonstration of treatment benefits." 29 Neurosurgeon Jose Ochoa writes: "the cutaneous territory affected by sensory symptoms exhibits matching (temperature) abnormality… (and is) indicative of sympathetic vasomotor unbalance."30 He also states (with Bill Triplett): "At present, thermography is the most valuable test available for evaluating the autonomic nervous system."31 Margaret Abernathy, MD, Editor of Thermology, views thermography as "A window on the sympathetic nervous system." 32
THEORY AND PRACTICE IN THERMOGRAPHIC INSTRUMENTATION
Contacting Instruments (Thermocouple, Thermistor, etc.)
Both Dossa Evan's Neurocalometer (NCM) and the early Chirometer employed differentially connected thermocouple elements mounted two inches apart on a sensing head.1 To examine a subject with these instruments, the sensing head is centered with moderate pressure on the spine at S2 and moved slowly to C1. If there is no side-to-side temperature difference, the voltage output remains zero. Similar operation is also described in literature for the non-recording "Nervo-Scope" and "Temp-o-scope."5,33 Because these differential instruments don't display actual temperatures, no indication is provided showing which side of the paraspinal skin surface is hotter or colder than normal. 5 Skin contacting instruments require good heat conduction between the epidermis and the thermal-sensing elements. Moving thermocouples can't "dwell" for several time constants at each point of interest, so thermal "lag" will occur. In addition, contacting instruments may create measurement error due to:
1. Inadequate heat exchange between the skin and the temperature detector; 2. Variations in glide speed; 3. Combined mechanoceptive and thermoceptive neuronal function which tends to rapidly alter skin temperature; 4. Non uniform pressure; 5. Inadequate "dwell" time; 6. Path-of-travel variations; and 7. Non uniform starting and ending points. Also, the temperature information from such instruments may be difficult to interpret or compare with the results of earlier examinations.
1,3,5,34
Non-Contacting Instruments (Infrared Radiation)
Non-Contacting temperature instruments sense variations in the quantity of heat radiated from the surface of interest. All objects above absolute zero (-273°ree Celsius) exchange radiant heat with hotter or colder objects in the direct line-of-sight. The rate of heat exchange between two objects depends upon: 1. Their absolute temperature difference; and 2. Their individual thermal emissivity. The "gold standard" heat emitter is a perfectly smooth dull-black body. This body has an emissivity of "1" because it absorbs all radiated heat.34 Electromagnetic waves are radiated at many frequencies. Microwave, heat and light frequencies overlap. Human thermoceptors and optical rods and cones combine to sense radiated heat and light energy ranging from 0.3 to nearly 100 microns(10-6 meters) in wavelengths. Visible-light (the higher frequencies) ranges between 0.38 microns for violet and 0.76 microns for deep red. Infrared radiation covers the remainder of the heat spectrum up to wavelengths of 100 microns. Heat radiated from human skin at 37°reeC (98.6°ree F) has a wavelength of approximately 9.3 microns, which is within the "near infrared" region of the electromagnetic spectrum. Normal, healthy human skin has an emissivity of approximately 0.97 +/- 0.01, which means that it is a good heat absorber or emitter. 3,34
To avoid sensing light radiation, optical filters that limit sensitivity to the 8-12 micron range should be employed with thermal sensors for human skin. Some thermal detectors are held at a very-low, constant temperature by immersing the case in boiling liquid nitrogen or argon. This increases detector sensitivity and provides a known-temperature reference. Commercial noncontacting, vapor deposited infrared detectors:
1. Require no surface contact; 2. Respond rapidly to temperature changes; and 3. Use microscopic thermocouple junctions that facilitate "thermopile" construction to gain high thermal sensitivity.3,35-37 "Spot" infrared radiometric instruments are common in chiropractic. They measure the infrared electromagnetic energy emitted from a localized area or territory (often a flat, circular target). The field of view usually forms a cone in front of the detector. Unless all objects within the measured target territory have the same temperature, however, the quantity of heat detected will change with distance to the targets.38-40 A spot radiometer that incorporates a focusing lens and collimating-barrel combination can limit the field of view to a small, almost constant-diameter target. A fresnel focusing lens may be used to direct most of the heat energy received to the relatively small heat detection surface inside the infrared detector. 3,41 When a precision infrared detector is moved over the skin surface, the thermal data obtained can easily be converted into digital signals which in turn may be displayed on computer video monitors. If the detected field of view is limited, a representation of the thermal variations occurring along a narrow scan path can be graphically displayed as a color trace. Different color computerized overlay comparisonswith previous scans of the same territory may be presented to review the thermal history of the skin surface.
Imaging Radiometry
Various highly-sophisticated thermographic instruments have been developed to image the variations in radiant heat emitted from large surfaces. In one type of commercial instrument, a single, liquid-nitrogen-cooled, infrared detector receives the heat reflected from a set of "raster-scanning" mirrors or prisms.38,39 These rotating mirrors have an effect similar to a focusing lens/collimating barrel combination. A small, focused detection "spot" scans horizontally and vertically across the target surface, receiving infrared radiation. The radiated energy is converted into temperature data which is stored, processed and displayed by a computer which presents it in the form of contoured thermal "images" of various colors. Each 1°ree C increment (sometimes less) of temperature is displayed as a different color or shade, resulting in a contoured image on a video monitor which represents a thermal "map" of the surface being scanned. Various thermographic instruments operating on these principles are used in chiropractic and medicine for diagnostic and outcome evaluations. The most expensive present color-graphic or grey-scale highresolution or low resolution images while others offer colored thermal traces which may be overlaid to assess progress.38-55 The Neurocalometer provided an essentially infinite temperature resolution. If a compromise of 0.3°reeC thermographic resolution is assumed to be suitable for precision chiropractic paraspinal analysis, however, at least 15 colors are needed to present a typical fullback image. This large number of colors may make interpretation of thermal anomalies quite difficult. Grey-scale data presentations offer increased resolution, but still require precision imagers and well trained interpreters. Conversely, computerassisted "spot" radiometry can produce thermal traces and images of relatively-high (0.05°ree C) resolution, making them more straightforward to interpret.
Thermographic Radiometric Instrumentation
Two types of non-contacting computerized infrared instruments which illustrate variations in non-contact thermographic technology are:
1.Multi-channel low-resolution spot radiometers with 12 infrared detectors mounted at 1-inch increments on a horizontal frame (VISI-THERM II)42; and 2.Cryogenic-cooled-detector thermal-imaging cameras (inframetrics, Agema, Mikron, etc.)43-49
Other non-contacting thermographic instruments include the Derma Thermograph,6,50 Pyroelectric Videcons51 and Charge- Coupled Devices. (Liquid-Crystal and NCM-type thermographic instruments are also available, but these are contacting devices which may create artifacts by eliciting sympathetic dermal vasomotor function.)52-54 Many of the thermographic instruments referenced here were recently reviewed in Chiropractic Products.55
THERMOREGULATION AND THERMOGRAPHY
The Physiology of Thermoregulation
Thermography images the status of dermal thermoregulatory function. Regulation of core temperature for body-heat maintenance is believed to be primarily a hypothalamic function. Local thermoregulation within each spinal dermatome is held to be modulated by spinal neuronal function.9 Present theory assumes that temperature anomalies in the paraspinal skin surface arise principally from variations in segmental (local) thermoregulation. Dermatomal anomalies are therefore hypothesized to arise from lesion or other non-uniform conditions within the involved body segment. As illustrated in Figure 1, hypothalamic "background" thermoregulation establishes the "set point" for body core-temperature (typically 37°ree C). The hypothalamic temperature "set point" tends to remain very constant for each individual, normally varying only slightly and slowly in daily and seasonal rhythms.56,57 In response to pathophysiological alteration, however, this body-temperature "set point" may vary instantly and significantly. An example is fever, which may be produced almost instantly in response to an infectious insult.58
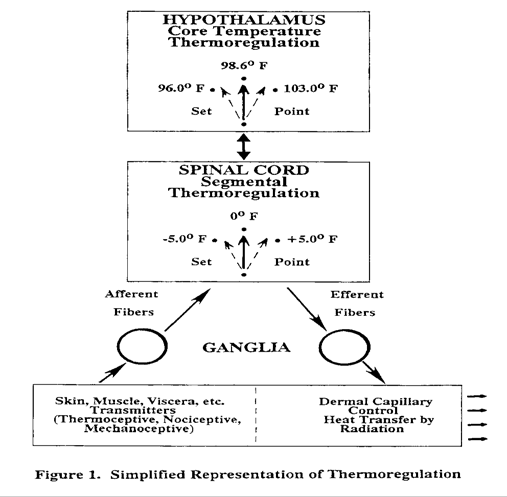
Hypothalamic/Spinal Thermoregulatory Relationships
Thermogenesis, which is mainly visceral, is known to be regulated by sympathetic spinal neuronal function under the influence of hypothalamic thermoregulation. Normally, core temperature is held essentially constant by the modulating function of sympathetic spinal nerve-cell bodies located between T2 and L2. Heat generated as the blood flows through the heart, liver and kidneys provides the major contribution to core heat. Regulation of skin surface radiation is the main controlling mechanism for preservation or dispersion of this core-heat. Spinal nerve-cell bodies control core temperature by regulating the dilation or constriction of the arterioles and capillaries within the innervated dermatome.3,56-58 The setpoint of hypothalamic "background" temperature can be inferred from oral, rectal or tympanic thermometry. This set point, however, is refined at each spinal segment by thermoregulative "C" sympathetic nerve cell bodies. Local, seg-mental thermoregulation by spinal cell bodies was shown to function even in the absence of hypothalamic input in decerebrate rabbits.60 Spinal nerve-cell bodies respond to thermoceptive, nociceptive and mechanoceptive afferents within their respective (and sometimes adjacent) dermatomes. During segmental nociception, this spinal modulation increases local skin temperatures, sometimes by as much as 5°reeC above the temperature of adjacent dermatomes. These thermoregulatory phenomena were validated by a number of investigators who studied animal and human neuronal function during the 60s and 70s.60-67 In cases of reflex sympathetic dystrophy and similar dysfunction, segmental thermoregulation modulates local skin to below the core temperature. In rare cases, skin temperatures have even appeared to be below normal room temperature without sweating effects.68-70
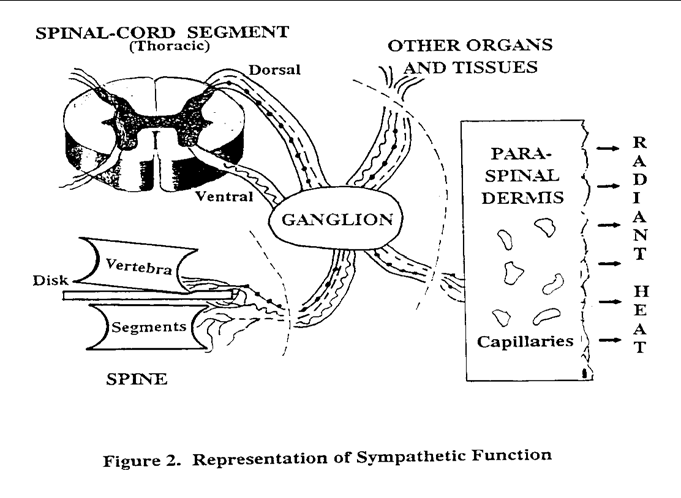
Typically, in each dermatomal segment, efferent axons extend from the thermoregulatory spinal-cord "C" cell bodies to the paraspinal ganglions. At the ganglions, these neurons synapse with post-ganglionic thermoregulative efferents, some of which terminate cutaneously. Cutaneous thermoregulatory function may occur in sympathy with noxious inputs from the same dermatomal segment (such as might be elicited by the VSC). Cutaneous sympathetic thermoregulatory neuronal function regulates vasomotor activity within the dermal arterioles and capillaries. Vasodilation tends to increase skin temperature, resulting in a greater heat transfer rate to the surrounding environment. Conversely, vasoconstriction causes the skin to approach ambient temperature, tending to conserve core heat.58
Simplified Physiology of Thermographic Findings
Segmental thermoceptive spinal nerve cell body function was found to almost instantaneously modify the local temperature set point after a pathophysiological alteration such as a spinal insult or adjustment. The result is rapid skin-temperature changes within the involved segment(s).9,58 Both thermoceptive and nociceptive responses may be referred by sympathetic fiber function to uninvolved dermatomal sites. Whether or not pain is involved, vasodilation within the dermal papillary beds is a common result, tending to create "hot" thermographic findings within the involved half of the dermatome. If there is no correction of the lesion, vasodilation often gradually decreases. After a period of months, vasoconstriction may begin and the dermis in the involved half-segment tends toward ambient temperature, resulting in significant "cold" thermographic findings.71 Cutaneous skin-temperature anomalies over dermatomal trigger points were found to be generally unrelated to local deep-tissue lesion. 72,73 Viscera, muscle, ligament, joint, synovia, even nerve-tissue organs all have sympathetic "somatocutaneous" zones which may change thermally during nociception. The immediate thermographic result is usually "hot", and may occur simultaneously in several cutaneous territories. If the lesion persists over a long period without correction, such as is common with a VSC, "cold" thermographic findings may eventually result. Although the presence of multiple anomalies in thermographic findings suggests pathophysiological alteration, the practitioner's responsibility is to isolate lesion location and severity.
Clinical thermography is based primarily upon four related hypotheses:
1.Skin-temperature regulation is segmental at the spinal dermatome level;
2.Spinal cell bodies modulate hypothalamic thermoregulation;
3.Remote lesion (including a VSC) generally creates asymmetrical sympathetic paraspinal skin temperature variations; and of special interest to chiropractic,
4.Significant temperature deviations from right-left symmetry or a uniform increase from sacrum to atlas suggest abnormal conditions.30,58
It is assumed that in properly stabilized subjects, abnormal thermographic findings result primarily from variations in alphareceptor regulation of skin papillary bed circulation. Lacking neurochemical involvement, these alpha receptors are responding to post-ganglionic fiber function under the direct influence of pre-ganglionic spinal nerve-cell-fibers in the involved dermatome. In essence, thermographic clinical analysis measures the physiological status of post-ganglionic fibers and their alpha-receptors. Under these assumptions, cutaneous temperature responses typically denote:
1.Thermographically "Hot"
•Decreased sympathetic-fiber function •Neurochemical alpha-receptor blockade
2.Thermographically "Cold"
•Increased sympathetic-fiber function •Increased alpha-receptor sensitivity 9,58
Functional Illustration
In the simplified illustration of figure 2, a thoracic VSC elicits nociceptive neuronal function that passes through the ganglion to the dorsal and ventral horns at the spinal cord. The elicited autonomic spinal-cord nerve cell function vasodilates skin capillaries. This vasomotor function results in a localized temperature increase, primarily within the involved right half of the dermatome. (Internuncial neuronal function at the spinal cord may result in similar but lower temperature increases within the left half of the elicited dermatome.) The higher blood-flow rate in right half cutaneous territories typically results in increased radiant heat emission from the paraspinal surface. The side-to-side skin temperature differences become the thermal asymmetry that differential thermographic scanning systems detect and display. In addition, local paraspinal skin temperatures (especially at trigger points) within the involved segment will usually be higher than in the adjacent dermatomes. The result is vertical thermal anomalies that may be revealed either by a single-detector paraspinal scanner or by dual-detector and wide-area scanners that present absolutetemperature displays.
EXPERIMENTAL VERIFICATIONS
Physiological Findings
Innervation by sympathetic fiber within the intervertebral discs is a fairly recent discovery. This discovery, however, gives the essential support needed to justify paraspinal thermographic assessment of a VSC. Because intervertebral discs are innervated, they are able to elicit sympathetic nerve function which in turn creates paraspinal thermal anomalies.74-76 Malik Slosberg concluded that therapeutic manipulation had a definite effect upon spinal afferent inputs. Obviously, thermoceptive function elicited by a non-VSC lesion or other stressors may also produce paraspinal thermal anomalies. Although paraspinal thermal anomalies may be suggestive of various nociceptive conditions within the involved dermatome(s), these anomalies may often be suggestive of a VSC.77
Generalized Thermographic Findings
The experimental evaluations of both symptomatic and asymptomatic patients by Sumio Uematsu and others gives excellent support to the assumptions outlined previously.78-83 Well designed thermographic investigations by John Jinkins helped to isolate lumbar disc extrusion.84-85 Infrared mapping of the cerebral cortex confirmed that thermal anomalies suggest dysfunction.86 Thermographic analyses of breasts, extremities, forehead to back thermal ratio, etc., produced similar results.87-89 Many investigators performed experimental evaluations to quantify typical cutaneous thermal responses to internal and external challenges. In one study, nearly 40 minutes were required for the skin to return to normal temperature after severe hot and cold challenges on the lumbar-thoracic paraspinal skin and posterior thigh.90 When a hand was immersed in cold water, the skin temperature of the ipsilateral foot invariably dropped in temperature.91 Stimulation of spinalthalamic tract neurons in monkeys revealed various dermatomal sympathetic responses, further indicating that spinal nerve-cell fiber function refines hypothalamic function.92 Through experimental evaluation, investigators were able to establish a thermodynamic model for the skin. This model implies that thermoregulation is very dynamic, even under normal conditions. In nude subjects experiencing the moderate coldtemperature stress of room temperature (70-73°ree F), skin temperatures began to oscillate. These oscillations had an average period of 30 minutes (after an initial 30 minute equilibration). Under greater cold stress, similar oscillations occurred that were not always symmetrical from side-to-side. With stress applied, side-to-side and local temperature oscillations were dramatically higher in frequency for symptomatic than for asymptomatic patients. These and many of the studies referenced earlier tend to prove that normal thermoregulation is indeed symmetrical and that either horizontal or vertical asymmetry suggests lesion, stress or both.93, 95 Investigators who employed autonomic challenges report various abnormal thermographic findings thought to be related to sympathetic nervous system function.96-99 One author found discernible thermographic effects from low-frequency vibration induced upon the lumbar spine, a common hazard in many occupations.100 Another used computer-aided thermographic image subtraction to image large subcutaneous blood vessels. The exact location of large subcutaneous blood vessels is important in the analysis of high-resolution thermographs because they are likely to create small thermal anomalies which reflect no abnormality.101
Thermography Compared with other Diagnostic Modalities
Lawson Cannon reported a 90% sensitivity for thermography, higher than for CT, EMG and myelography. He also reported correlations between "other clinical findings" and thermography of between 93 and 100% for various experienced practitioners.12 Several authors who compared thermographic and other instrumental modalities, including: evoked potentials, myelography, electromyography, CT, MRI, and EIT, etc., found in most cases that good correlation existed between modalities.102-110 Chiropractic and medical literature detailing general clinical and individual case studies also give encouraging anecdotal evidence of the validity of thermography as an objective patient-assessment modality.111-123
Thermographic Analysis Protocols
To develop repeatable, scientifically-defensible assessment data, precision instrumentation should be combined with strict adherence to standardized test protocols and informed interpretation. If protocols aren't carefully established and followed, artifacts may be produced which are difficult to separate from useful data.124 Most thermographic protocols are similar in their requirements.125-127 A draft-free examining room is needed where the temperature is held within a narrow range [some recommend that the room be relatively cool (approximately 66-68°reeF) to create moderate thermal stress]. Some call for at least 15 minutes for equilibration during which skin surface to be scanned remains nude. Subject position, wall construction, stool height, same time of day for repeat examinations, psychological factors, etc., are all considered important. For at least 4 and up to 24 hours, subjects are encouraged to avoid eating, bathing, strenuous exercise or activity, nicotine, prescription drugs (especially pain medicine), skin ointments, and hot or cold caffeinated or alcoholic beverages. (All of these requirements aren't necessarily valid for chiropractic assessment.)
Based on present technology, cutaneous thermographic findings are a reflex of:
1.Segmental thermoregulation; 2.Core-heat thermoregulation; 3.Environmental exposure; 4.Physiological status; and 5. Individual-unique responses.
Abnormal paravertebral thermographic patterns may relate to either skeletal neuronal interference or to sympathetic response to a VSC or other nociceptive lesion in remote or local organs or tissue (or combinations of these conditions).30 Chiropractors report that paraspinal skin temperatures usually change immediately after a spinal adjustment, making thermography an effective clinical tool for patient assessment. "X-ray defines (anatomical) structure, MRI defines (body) chemistry, and Thermography is used to define (physiological) function,"states Rockley.128 (Emphasis added). Thermography provides a way to visualize spinal neuronal function, i.e., physiology. "…Thermography is often the only diagnostic test which can accurately measure the amount of musculoskeletal or neurological damage … setting the stage for an accurate diagnosis and prognosis."13 Whether or not pain is present, paraspinal thermography can reveal abnormal sympathetic nerve-fiber function which may in turn be indicative of the VSC.3 Infrared thermography is one of the few diagnostic tools which may be used repeatedly with no known hazard to the patient. It also has important legal implications, especially in the establishment of need for treatment and confirmation of injury.129,130
CONCLUSIONS
There is sound thermoregulative physiology to support paraspinal thermographic findings for clinical assessments, especially to help assess a VSC. To provide maximum benefit, computerized infrared paraspinal thermography should present "heat only" data, have high thermal resolution and produce repeatable scan-to-scan data. Also, permanent recording of all significant scan data and user-friendly operation which integrates well with typical clinical and clerical office routines are essential. Paraspinal thermography has been a useful diagnostic test for remote lesion within an involved body segment. There is a need for further scientific investigative effort to provide additional support for the major premise of this paper, i.e, anomalies in sympathetic spinal thermo-regulation are often suggestive of the VSC because sympathetic spinal cell-body function modulates hypothalamic control. Chiropractic has long pursued the highest-possible objectivity in the validation of its spinal assessment and adjustment procedures. More general use of high-resolution, high-accuracy computerized thermography could produce significant improvements in health care and advance the entire profession.
Acknowledgments:
The authors wish to thank Drs. Donald Kern, Robert Wagnon, James Wood and Charles Henderson of the Palmer College Institute
of Graduate Studies and Research for their valuable assistance in the preparation of this article.
REFERENCES
1.Palmer, BJ. Precise posture spinograph comparative graphs. Palmer School of Chiropractic Press, 1938. 2.Dye AA. The evolution of chiropractic. Richmond Hall 1939. 3.Christiansen J, Gerow G. Thermography. Baltimore: Williams & Wilkins 1990:. 4. Resh, RE. NeuralScan- a window into the spine. unpublished brief, 1992. 5.Herbst, RW. Chiropractic science and healing art. Gonstead SCI CHI 1980; 160-163. 6.Pierce, WV. Results. Dravosburg PA. X-Cellent X-Ray Company 1986. 7.Kern, DP. Pattern system theory of skin-temperature analysis. Private Communication, unpublished brief, 1992. 8.Korr, IM, et. al. Effects of experimental myofascial insults on cutaneous patterns of sympathetic activity in man. Journal of Neural Transmission 1962; 23:22:330-355. 9.Simon EK. Temperature regulation-spinal cord as a site of extrahypothalamic thermoregulation functions. Reviews of Physiology, Biochemistry and Pharmacology 1975;71:1-76. 10.Meeker, WC, Gahlinger, PM. Neuromusculoskeletal thermography; a valuable diagnostic tool? Journal of Manipulative and Physiological Therapeutics 1986; Dec 9:4:257-266. 11. Kent, C, Daniels, J. Chiropractic thermography: a preliminary report; International Review of Chiropractic 1974; Nov 4-23. 12. Cannon L. The validation of thermography. American Chiropractor 1987; Feb 12-26. 13.Cockburn W. The current state of thermography. Today's Chiropractic May/June 1988; 17:3:67-69. 14.Diakow, PRP, et. al. Correlation of thermography with spinal dysfunction: preliminary results. The Journal of the Canadian Chiropractic Association 1988; June 32:2:77-80. 15.Hubbard J. Neuromuscular thermography: an analysis of criticisms. Thermology 1990;3:160-165. 16.Walklett W, Green J. Heat as a diagnostic aid. Administrative Radiology 1990 March ;57-9. 17.Green, J. Neurothermography. Seminars in Neurology 1987; Dec 7:4:114-117. 18.Wexler, CE. An overview of liquid crystal and electronic lumbar, thoracic and cervical thermography. Tarzana California Thermographic Services, 1983. 19.Carter, LM. The clinical role of thermography. Journal of Medical Engineering and Technology 1978; May 2:3:125-128. 20.Pochaczevsky, R. The value of thermography as a clinical imaging diagnostic test; a review of and response to the 1989 office of health technology assessment report of thermography for indications other than breast lesions. Thermology 1991; 3:227-233. 21.Pochaczevsky, R, et. al. Liquid crystal thermography of the spine and extremi-ties. Journal of Neurosurgery 1982; March 56:386-395. 22.Rothschild, BM. Thermographic assessment of bone and joint disease. Orthopedic Review 1986; 15:12:33-48. 23.BenEliyahu, DJ. Infrared thermal imaging of the vertebral subluxation complex. ICA International Review of Chiropractic 1992; Jan/Feb 14-17. 24.Awerbuch, MS. Thermography – its current diagnostic status in musculoskeletal medicine. The Medical Journal of Australia 1991; April 154:441-444. 25.Stillwagon G, Stillwagon K. Computerized infrared thermography. Today's Chiropractic 1985; 14:28-9. 26.Stillwagon. G. et. al. Chiropractic thermography. ICA International Review of Chiropractic Jan 1992; 8-13. 27.BenEliyahu DJ. Thermography in clinical chiropractic practice. ACA Journal of Chiropractic 1989; Aug 59-72. 28.Conwell TD. Musculoskeletal thermography, a literature review. Colorado Chiropractor, 1989 March/April Part 1, May/June Part 2. 29.Hobbins WB. Thermography-neurophysiology and chiropractic. Today's Chiropractic 1989; June 42-4. 30.Ochoa J, et al. Mechanisms of neuropathic pain: cumulative observations, new experiments, and further speculation. Advances in Pain Research and Therapy 1985;9:431-450. 31.Triplett, BR, Ochoa, J. Contemporary techniques in assessing peripheral nervous system function. Journal of EEG 1990;24:29-44. 32.Abernathy M. Thermography: a window on the sympathetic nervous system. Thermology 1988; 1:4,5. 33.Cox, WA The Gonstead Technique. Today's Chiropractic 1986. May/June 75,76,115. 34.Shortly, G, Williams, D. Elements of Physics. Prentice Hall, NY, 1953; 254-259. 35.Optek. Infrared sensors, Optek Technology. Carrolton, TX 1992. 36.Murata Erie. Pyroelectric Infrared Sensors-IRA Series. Smyrna, GA. 1992. 37.Honeywell, Microswitch. Optoelectronic Sensors. Freeport, IL. 38.Astheimer, RW. Infrared to visible image translation devices. Photographic Science and Engineering 1969; May/June 12:3:127-133. 39.Clark, RC. A technical view of medical infrared thermography. unpublished paper. 40.Rockley, GJ, Rockley, MG. Breakthroughs in computer-assisted thermal imagers. Today's Chiropractic 1990; May/June 55-57. 41.Titone, R. Thermographic Instrumentation. The American Chiropractor 1992; July/ Aug 32-38. 42.Visi-Therm, Visi-Therm by SSI, Monongahela, PA. 43.Inframetrics Forensic Special, Inframetrics, Bedford, MA. 44.Neurothermography. Bales Scientific Inc. Walnut Creek, CA 45.Dorex, Dorex Computer Aided Thermography Systems, Orange, CA. 46.Probeye, MC Sales Inc, Oregon, WI. 47.Agema Infrared Systems, Agema, Secaucus, NJ. 48.Mikron Thermo Tracer, Mikron, Wyckoff, NJ. 49.Thermal Video System, Nippon Avionics, Cincinnati Electronics Corp, Mason, OH. 50. Kimmel, EH. The derma thermograph. Journal of Clinical Chiropractic 1969. Feb 2(4)77-86. 51.80 Series Thermal Imaging System, Insight Vision Systems Inc, Kensington, MD. 52.NovaTherm, Med Tech Products Inc, Dayton, OH. 53.Sinotest & Cont- Flex Systems, International Products & Services, Milan, Italy. 54.Mark V Thermography, Flexi-Therm Inc, Westbury, NY. 55. The imaging companies. Chiropractic Products 1989; Aug 68-101. 56.Bentzinger, TH, Heat regulation: Homeostasis of central temperature in man. Physiological Reviews, The American Physiological Society 1969; 49(4)671-752. 57.Gardner, E, Bunge, RP. Gross Anatomy of the Peripheral Nervous System, Peripheral Anatomy. WB. Saunders 1984; 1:11-38. 58.Hobbins WB. Scientific basis of thermography. Director's Line 1990. 59.Ochoa, J. Unmyelinated fibers, microneurography, thermography and pain. AEEE Course B, Ochoa. 1986 29:32. 60.Chai, CY. Lin MT. Effects of thermal stimulation of medulla oblongata and spinal cord on decerebrate rabbits. Journal of Physiology 1973; 242:409-419. 61.Inoue, S, Murakami, N. Unit responses in the medulla oblongata of rabbit to changes in local and cutaneous temperature. Journal of Physiology 1976. 62.Chai, CY. Lin MT. Effects of heating and cooling the spinal cord and medulla oblongata on thermo- regulation in monkeys. Journal of Physiology; 1971 225:297-308. 63.Bacon, M, Bligh, J. Interaction between the effects of spinal heating and cooling and of injections into a lateral cerebral ventricle of noradrenaline, 5-hydroxytryptamine and carbachol on thermo- regulation in sheep. Journal of Physiology 1976; 254:213-227. 64.Banet, M, et. al. Autonomic thermoregulation after intermittent cooling of the spinal cord and cold exposure in the rat. Journal of Physiology 1978; 275:439-447. 65.Husstedt, IW, et. al. Standardization of neurophysiological norm values, Relevance of the position of the heating element and the temperature measurement sensor; Electromyographic Clinical Neurophysiology 1991; 31:61-64. 66.Guieu, JD. Hardy, JD. Effects of preoptic and spinal cord temperature in control of thermal polypnea. Journal of Applied Physiology 1970; April 28(4)540-542. 67.Kodsoka, M, et. al. Effect of thermal stimulation of spinal cord on respiratory and cortical activity. American Journal of Physiology 1969; 297:3:858-863. 68.Edwards, BE. Reflex sympathetic dystrophy since Livingston. Thermology 1988; 3:59-61. 69.Hershey, LA, et. al. Computerized thermography in post-stroke reflex sympathetic dystrophy. Thermology 1988; 3:62-65. 70.Ring, EFJ, et. al. Reynaud's phenomenon: assessment by thermography. Thermology 1988; 3:69-73. 71.Pulst, M, Haller, P. Thermographic assessment of impaired sympathetic function in peripheral nerve injuries. Journal of Neurology 1981; 226:35-42. 72.Fischer AA, Chang CH. Temperature and pressure threshold measurements in trigger points. Thermology 1986; 1:212-5. 73.Kruse RA, et al. Thermographic imaging of myofascial trigger points. American Journal of Chiropractic Medicine 1990: June 3(2)67-70. 74.Bogduk N, et al. The innervation of the cervical intervertebral discs. Spine 1989; 13:1. 75.Bogduk N. The innervation of the lumbar spine. Spine 1983;8:286-93. 76.Edgar,
MA, Ghadially, JA. Innervation of the lumbar spine. Clinical Orthopedics and Related Research 1976; Mar/Apr 115:35-41. 77. Slosberg, M. Effects of altered afferent articular input on sensation, proprioception, muscle tone and sympathetic reflex responses. Journal of Manipulative and Physiological Therapeutics 1988: Oct 11:5:400-408. 78.Uematsu S, et. al. Quantification of thermal asymmetry-part 1; normal values and reproducibility. Journal of Neurosurgery 1988; October 69:552-555. 79. Uematsu S, et. al. Quantification of thermal asymmetry-part 2; application in low back pain and sciatica. Journal of Neurosurgery 1988; October 69:556-561. 80.Uematsu S. Symmetry of skin temperature comparing one side of the body to the other. Thermology 1985; 1:4-7. 81.Goodman PH, et al. Normal temperature asymmetry of the back and extremities by computerassisted infrared imaging. Thermology 1986;1:195-202. 82.Green J, et al. Abnormal thermographic findings in asymptomatic volunteers. Thermology 1986;2:13-5. 83.Roberts, WJ, Foglesong, ME. A neuronal basis for sympathetically maintained pain. Thermology 1986; 2:2-6. 84.Jinkins, JR. The anatomic basis of the autonomic syndrome associated with lumbar disk extrusion. Thermology 1990; 262-272. 85.Jinkins, JR, et.al. The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. American Journal of Roentgenology 1989; 152:277-289. 86.Gorbach, AM, et. al. Infrared mapping of the cerebral cortex. Thermology 1989; 3: 108-111. 87.Ishigaki, T. Forehead-back thermal ratio for the interpretation of infrared imaging of spinal cord lesions and other neurological disorders. Thermology 1989; 5:101-107. 88.Dodd, GD, et. al. Thermography and cancer of the breast. Thermology 1988; 3:74-78. 89.Harway, RA. Precision thermal imaging of the extremities. Orthopedics 1986; March 9(3)379-382. 90.Goodman, PH, et. al. Detection of intentionally produced thermal artifacts by repeated thermographic imaging. Thermology 1991; 3:253-260. 91.Uematsu S, Jankel WR. Skin temperature response of the foot to cold stress of the hand: a test to evaluate somatosympathetic response. Thermology 1988; 3:41-9. 92.Bolser, DC, et.al. Convergence of phrenic and cardiopulmonary spinal afferent information on cervical and thoracic spinothalamic tract neurons in the monkey: implications for referred pain from diaphragm and heart. Journal of Neuropathy 1991; May 65(5)1042-1044. 93. Boesiger P, Geser HM. A thermodynamic model for thermographic analysis of tissue perfusion and its regulation. Thermology 1990;3:191-8. 94.Roberts DL, Goodman PH. Dynamic thermoregulation of back and upper extremity by computer-aided infrared imaging. Thermology 1987;2:573-7. 95.Anbar, M, et.al. Manifestation of Neurological abnormalities through frequency analysis of skin temperature regulation. Thermology 1991; 3:234-241. 96.Hobbins, WB. Autonomic challenge test. unpublished paper. 1985. 97.Ochoa, J, Torebjork, E. Sensations evoked by intraneural microstimulation of C nociceptor fibres in human skin nerves. Journal of Physiology 1989; 415:583-599. 98.Charny, CK, et. al. A whole body thermal model of man during hyperthermia. IEEE Transactions on Biomedical Engineering 1987; 34(5)375-387. 99.Frost, SA, et. al. Does hyperalgesia to cooling stimuli characterize patients with sympathetically maintained pain (reflex sympathetic dystrophy)? Proceedings of the World Congress on Pain, 1988; Elsevier Science Publishers BV (Biomedical Division). 100.Konerding, MA, et.al. Effects of whole-body vibration on the lumbar vertebral column: experimental infrared thermographic studies. Thermology 1990; 3-177-181. 101.Chan EKY, Pearce JA. Visualization of dynamic subcutaneous vasomotor response by computer-assisted thermography. IEEE Transactions on Biomedical Engineering Aug 1990;37(8)786-94. 102.BenEliyahu DJ, Silber BA. Infrared thermography and magnetic resonance imaging in patients with cervical disc protrusion. American Journal of Chiropractic Medicine June 1990;3:2. 103. BenEliyahu DJ. Thermography: the significance of CT/MRI documented disc bulges and herniations. Today's Chiropractic Aug 1990. 104.Goldberg GS. Infrared imaging and magnetic resonance imaging correlated in 35 cases. Thermology 1986;1:207-11. 105.Hubbard JE, Hoyt C. Pain evaluation by electronic infrared thermography: correlations with symptoms, EMG, myelogram and CT scan. Thermology 1985;l(l)26-35. 106.Conway J, et al. An experimental study of electrical impedance tomography (EIT) for thermal monitoring in the human body. Thermology 1990;3:182-6. 107.Chafetz N, et al. Neuromuscular thermography of the lumbar spine with CT correlation. Univ of California Dept of Radiology, San Francisco 94143. 108.Glick DM, Lee F. Differential diagnostic somatosensory evoked potentials. Chiropractic Research Journal 1991; 2(2)38-47. 109.Fischer AA, et.al. Correlation between thermographic findings and somatosensory cortical evoked potentials in lumbrosacral radiculopathies. Thermology 1986; 2:29-33. 110.BenEliyahu DJ. Thermography in the diagnosis of sympathetic maintained pain. American Journal of Chiropractic Medicine 1989; June 2(2)55-60. 111.Gerow G, et.al. Thermographic Evaluation in a patient with a lumbar disc herniation. Today's Chiropractic 1990; Sep/Oct 72-74. 112.Forster G. Thermographic appearance of multiple level cervical stenosis – a case study. Review 1990; Winter 24-5. 113.BenEliyahu DJ. Infra-red thermographic assessment of chiropractic treatment in patients with lumbar disc herniations – a clinical study. Proceedings of the 1990 International Conference on Spinal Manipulations, FCER May 11-12,1990; 405-411. 114.Harris W, Wagnon RJ. The effects of chiropractic adjustments on distal skin temperature. J Manipulative & Physical Therapy 1987; 10:2:57-60. 115.Ishigaki T, et.al. Infrared imaging of spinal cord lesions: relation between thermal abnormalities and extent of the lesion. Thermology 1987;2:578-83. 116.Farris HW. Thermography in
evaluation of nerve root fiber dysfunction. The American Chiropractor 1988; June 58. 117.Diakow RP. Thermographic assessment of sacroiliac syndrome: report of a case. The Journal of the Canadian Chiropractic Association Sept 1990; 34:3:131-134. 118.Leroy PL, et.al. Diagnostic thermography in low back pain syndromes. Clinical Journal of Pain 1985;1:4-13. 119.Wexler C. Diagnosing spinal problems with thermography. Flexitherm Inc. Westbury NY 11590. 120.Ignacio D, et.al. Thermographic monitoring of sympathetic nerve block. Thermology 1986; 2:21-24. 121.E]ias WV, et.al. Screening thermography of chronic back pain patients with negative neuromusculoskeletal findings. Thermology 1989; 3:125,126. 122.So YT, Aminoff MJ, Olney RK. The role of thermography in the evaluation of lumbo-sacral radiculopathy. Neurology Sept 1989; 1154-1158. 123. BenEliyahu DJ. Thermography in the diagnosis of sympathetic maintained pain. American Journal of Chiropractic Medicine 1989; June 2(2)55-60. 124.Anbar M. Potential artifacts in infrared thermographic measurements. Thermology 1991; 3:273-274. 125.Protocol for Clinical Thermography, Digest of Chiropractic Economics 1991; Sep\Oct 60-63. 126.Technical Guidelines, Edition 2. Thermology 1986;2:108-12. 127.Feldman F, Nickoloff EL. Normal thermographic standards for the cervical spine and
upper extremities. Skeletal Radiology 1984; 12:235-249. 128.Rockley MG. Advancements in the imaging field of telethermography. American Chiropractor 1988; Sept 6&8. 129.Chapman GE. Thermography and pain syndromes: analysis and medical legal implications. Chiropractic Products 1989; Aug 91-96. 130.Rein H. Thermography: medical and legal implications. American Chiropractor 1986: June 7,8.