Thermal Imaging in the Investigation of Deep Venous Thrombosis

Harding, J. Richard. St. Woolos Hosp., Newport (U.K.)
Preliminary assessment of clinically suspected deep venous thrombosis (DVT) of the lower limb by thermography avoids the need for over one third of venograms or duplex Doppler ultrasound scans.
Clinical diagnosis of DVT is notoriously unreliable – hence the need for an accurate means of clinical investigation. Untreated DVT is dangerous as it can progress to pulmonary embolism (PE) which is frequently fatal or life-threatening. Treatment of DVT by anticoagulation poses risks of its own however, and should not be undertaken without a confirmed diagnosis. Thermal imaging is quick, simple, non- invasive, risk-free, cost-effective and highly sensitive in the initial investigation of suspected DVT; a negative thermogram excludes DVT and avoids the necessity for further investigation. Thermal imaging is, however, non-specific; a positive thermogram has a number of possible causes and is an indication for further assessment by venography or Doppler ultrasound to confirm or exclude DVT. Thermography should be considered the initial investigation of choice in clinically suspected DVT, proceeding to venography or Doppler ultrasound only when thermography is positive.
INTRODUCTION
Deep venous thrombosis (DVT) poses an important diagnostic challenge in medical practice. Along with secondary pulmonary embolism (PE), DVT is a significant cause of emergency hospital admission, and also occurs in patients already undergoing hospital in-patient investigation or treatment; post-operative patients and those suffering from malignant disease (especially abdominal and pelvic malignancy) are particularly at risk. The major complication of DVT is of fragments of blood clot (thrombi) becoming detached (emboli) and passing through the veins of the lower limb, the inferior vena cava, and the right atrium and right ventricle of the heart into the pulmonary arterial circulation of the lungs where they become lodged in, and occlude branches of the pulmonary arterial tree as pulmonary emboli causing pulmonary infarction of the distal perfused pulmonary tissues. This is a serious and life-threatening event immediately fatal in 30% of cases [1]. Fatal pulmonary embolism causes over 20,000 deaths annually in Great Britain and accounts for 10% of all deaths in hospital [2]. DVT is treated by anticoagulation; this treatment has risks, in particular haemorrhage, and is expensive and time-consuming and should not be undertaken without a confirmed diagnosis of DVT or PE. Clinical diagnosis of DVT is notoriously unreliable [2], hence the need for reliable investigations to confirm or exclude DVT.
The traditional method of investigation of DVT, still regarded as the "gold standard", is lower limb venography (phlebography)[3], which outlines the deep venous system of the lower limb with radiographic contrast medium giving excellent detail of anatomy and pathology. This suffers the disadvantages of being invasive, at best uncomfortable for the patient if not painful, with risks of allergy to intra-venous injection of contrast medium (at worst fatal), the potential of dislodging emboli from lower limb venous thrombi due to the forced volume injection of contrast, irritation of the venous endothelium by the contrast medium actually causing DVT when not already present, precipitation of cardiac failure in susceptible subjects due to the fluid load of hypertonic contrast medium drawing fluid into the vascular space, and exposes the patient to ionising radiation with its attendant risks. Venography is also expensive for consumable materials (mostly radiographic contrast medium and film).
Various other methods of investigation of DVT have been utilised including isotope scanning for lower limb thrombosis, light reflection rheography, impedance plethysmography and measurement of C reactive protein or fibrin degradation products, but none have gained widespread acceptance due to various drawbacks. In recent years, duplex Doppler ultrasound has gained popularity [4], replacing venography in many institutions, but it has the disadvantages of being time-consuming, operator dependent, interpretation being to some extent subjective, and exclusion of DVT confined to the calf veins can be difficult or impossible [5]. Thermography was first described in the investigation of DVT in 1972 [6]. It has been shown that thermographic investigation of DVT can avoid the need for further investigation by venography or duplex Doppler ultrasound [7]. Whilst thermography is non-specific, it has the advantage of being highly sensitive (approaching 100%) [8], and is non-invasive, risk-free, does not expose the patient to ionising radiation, is not operator dependent or subjective in interpretation, and it is simple, quick and cheap to perform.
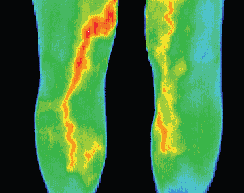
In acute DVT, the presence of propagating thrombus in the deep veins causes increased skin temperature in the affected lower limb due to the action of vaso-active amines on the capillary skin circulation [9]; thermal imaging detects this increased skin temperature along with loss of the normal 3oc temperature gradient down the affected lower limb [10]. The aim of this study was to prospectively assess clinically suspected DVT in order to determine what proportion of patients could avoid further investigation by virtue of normal thermography.
METHODS
1,000 patients with clinically suspected DVT were investigated by thermography by a single operator over a period of 6 years 3 months. Thermal imaging of the lower limbs was initially performed by liquid crystal thermography using the NovaTherm apparatus, followed by imaging with an Aga Thermovision 782 infrared camera. The lower limbs are first equilibrated with normal room temperature for 10 minutes by positioning the patient supine with both legs fully exposed and slightly elevated, with the heels supported, allowing free circulation of air over the skin, away from localised sources of heat or cold such as radiators, direct sunlight or draughts. Images are then obtained of the anterior aspect of both thighs, the antero-medial aspects of the calves, and the posterior calves.
RESULTS
There were 362 male (36.2% of total) and 638 female patients (63.8% of total). The males had an age range of 22-91 years and the females an age range of 15-96 years with a mean age of 65.0 years for males and 63.5 years for females.
Thermal imaging was not possible in two patients due to lack of patient co-operation. There was no difference in result in patients examined by both liquid crystal thermography and I-R thermography. Thermography was normal in 374 patients out of 1,000 (37.4%) i.e. no increased skin temperature or loss of the normal temperature gradient was demonstrated in the lower limb in which DVT was suspected; these examinations were thus negative for DVT and no further investigation was undertaken. There were no cases of clinically suspected or proven PE on follow-up of these patients. Of the 624 patients with increased temperature in the lower limb in which DVT was suspected, i.e. positive thermography, DVT was confirmed by venography and/or duplex Doppler ultrasound in 297 (47.6%), excluded in 211 (33.8%) and no further investigation was possible in 116 (18.6%), due to lack of accessible veins, patient refusal to undergo venography, unavailability of Doppler ultrasound in the earlier years of this study, or request for no further investigation to be undertaken by the referring clinician.
DISCUSSION
Thermal imaging avoided the need for further investigation by venography or duplex Doppler ultrasound in 37.4% of patients. Thermal imaging offers considerable financial savings over the more expensive conventional investigations which it has been demonstrated can be avoided in over one third of cases. By comparison with venography, thermography results in the most significant revenue savings, assessed at US $26,350 (Canadian $37,230) per 1,000 patients. This potential saving is of great importance to health providers with cash constraints. Compared with duplex Doppler ultrasound there is less financial saving, as thermography costs about half as much as Doppler for consumables, but there is considerable saving of skilled ultrasonographer and equipment time. Thermography has the advantage of being totally non-invasive and risk-free and quick and easy to perform. It is suggested that the ideal investigative pathway in clinically suspected DVT should be initial thermography, proceeding to Doppler ultrasound only when thermography is positive, and finally proceeding to venography only after negative or equivocal duplex Doppler ultrasound.
ACKNOWLEDGMENTS
Financial support has kindly been provided by The U.S. Department of Defense Agencies. I am indebted to Professor E F J Ring, Royal National Hospital for Rheumatic Diseases, Bath, UK, for the provision of an Aga Thermovision 782 I-R thermal imaging camera.
REFERENCES
1 Benotti JR, Ockene IS, Alpert JS, Dalen JE. The clinical profile of unresolved pulmonary embolism. Chest 1983;84:669-78.
2. Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med 1989;82:203-5.
3. Lea Thomas M. Phlebography of the lower limb. Edinburgh: Churchill Livingstone, 1982.
4. Nicolaides AN, Renton SC. Duplex scanning: the second sight of the vascular surgeon. Eur J Vasc Surg 1990;4:445-7.
5. Mitchell DC, Grasty MS, Stebbings WSL, Nockler IB, Lewars MD, Levison RA et al. Comparison of duplex ultrasonography and venography in the diagnosis of deep venous thrombosis. B J Surg 1991;78:611- 3.
6. Soulen RL, Lapayowker MS, Tyson RR, Korangy AA. Angiography, ultrasound and thermography in the study of peripheral vascular disease. Radiology 1972;105:115-9.
7. Gordon YB, Cooke ED, Bowcock SA, Ratky SM, Pilcher MF, Chard T. Non-invasive screening for venous thromboembolic disease. Br J Haematol 1977;35:505-10.
8. Pochaczevsky R, Pillari G, Feldman F. Liquid crystal contact thermography of deep venous thrombosis. AJR 1982;138:717-23.
9. Cooke ED, Pilcher MF. Deep vein thrombosis: preclinical diagnosis by thermography. Br J Surg 1974;61:971-8.
10. Stevenson AJM, Moss JG, Kirkpatrick AE. Comparison of temperature profiles (Devetherm) and conventional venography in suspected lower limb thrombosis. Clin Radiol 1990;42:37-9.