X-Ray Vision in Hindsight
February 11, 2002
Science, Politics and the Mammogram
By GINA KOLATA and MICHAEL MOSS
For decades, it was an article of medical faith: Get a mammogram; it could save your life.
Now, seemingly overnight, that faith has been shaken. The mammogram — that yearly ritual for millions of American women — has become the focus of a bitter and unusually public scientific dispute that is being fought in the pages of medical journals and the columns of daily newspapers. Scientists, policy makers and politicians have scheduled meetings and Congressional hearings. In the end, though, there is not likely to be a quick answer to the central question of whether researchers were right when they said that screening healthy women reduces death from breast cancer or, to put it another way, whether women should still get that annual mammogram.
"What a mess, what a complete mess," said Cindy Pearson, executive director of the Women's National Health Network, an advocacy group that has been flooded in recent days with phone calls from anxious women. "They want to know what is all this based on, is there some sort of sneaky, behind-the-scenes thing going on?" How that mess came to be is a story of science and politics and the business of medicine, and a war on cancer that seized upon mammography as a central weapon. It also is a story of the way science struggles toward an ever evolving "truth."
The mammogram has always been a modest weapon, with benefits that women must weigh against possible risks. It is a screening tool that misses some tumors. At most, studies have found, it can cut the breast- cancer death rate by 30 percent. Even when mammograms do "work," what they find does not always turn out to be cancer. The cancer they find may be growing so slowly that it would never threaten a woman's life. The result can be surgery, radiation and chemotherapy that is not medically necessary.
Over the years, scientists and statisticians have quietly debated the merits of mammography. Most of the public debate, though, has focused on its effectiveness for women in their 40's. That was already in considerable doubt when the larger issue broke open last fall with the publication of a study by a pair of researchers based in Denmark. They argued that the clinical trials most often cited to support mammogram recommendations were too flawed to be reliable. Last month, an influential but independent panel of experts at the National Cancer Institute agreed and said it could no longer make a recommendation about whether women should be screened. "These are huge issues," said Dr. Barnett Kramer, chairman of the panel and associate director of disease prevention at the National Institutes of Health. "They shake my confidence."
For its part, the cancer institute says that after reviewing the matter, it concluded that the new analysis did not refute evidence that mammography works, and that it is standing by its recommendation that women 40 and older be screened. Many of those who did the original trials are vigorously defending their work. While there are flaws in the studies, they say, the Danish analysis exaggerated their significance and misinterpreted facts. A number of experts agree. "I think the trials have imperfections," said Dr. Steven Woolf, a member of the United States Preventive Services Task Force, a panel that reviews scientific evidence about disease prevention. "But the issue is whether they invalidate the studies. My own view is that they do not rise to that level."
Since a new trial would require tens of thousands of women and a decade for results, some scientists are talking about digging deeper and more carefully into the old ones. Now, mammography supporters, led by the American Cancer Society, worry that the uncertainty will weaken the government's resolve. They say mammography is a leading reason that the breast-cancer death rate has been dropping for the last decade. Others, including those skeptical of mammography, ask whether the decline is a result of better treatments, especially the drug tamoxifen. For them, the furor is an opportunity to turn the focus of the war against breast cancer toward better treatment and the search for a cure.
A leading skeptic is Dr. Donald Berry, a medical statistician at the M. D. Anderson Cancer Center in Houston, where techniques were developed in the 1950's that spread mammography throughout the nation. Dr. Berry is a member of the federal advisory panel that is backing away from its support of mammography. "Breast people here think I'm doing a disservice to women, and I think they are doing a disservice to women," Dr. Berry says. "Who's right?"
A Eureka Moment
One evening in late 1970, Sam Shapiro took his research team to a Swiss restaurant in Manhattan, where he broke the news that transformed the medical and political approach to breast cancer. Dr. Philip Strax, a radiologist who had begun impressing surgeons by finding tumors before they could feel a lump, was at the table. To see if the mammograms really worked, Mr. Shapiro, the research director at Health Insurance Plan of Greater New York, had begun a scientific inquiry called a randomized trial. He divided women, ages 40 to 64, into two groups, and gave mammograms to just one. The study had paid off, Mr. Shapiro told his colleagues that evening. In the first seven years of the study, 81 of 31,000 women who had mammograms died of breast cancer, compared with 124 of 31,000 who were not screened, a difference in the breast cancer death rate of a little more than 30 percent.
"It was thrilling," recalls Dr. Raymond Fink, who was in charge of recruiting women for the study. It was, he adds, "one of those movie moments," like the scene in "The Story of Louis Pasteur" when Paul Muni says, "I found the germ!" Mammograms took off.
Before long, the National Cancer Institute, the American Cancer Society and other organizations issued guidelines telling women to have mammograms starting at age 40. The federal government advocated the breast X-ray like no other medical procedure. It pushed states to promote its use, compelled insurance companies to pay the bills and rode herd on the radiologists who did mammograms to ensure that they did a good job. Now, an estimated 30 million women are having annual mammograms, and many are having additional tests, like sonograms, when findings are suspicious. That leads to annual costs of more than $3 billion, said Dr. Martin L. Brown, an economist at the National Cancer Institute.
A Question of Age
From the start, there was concern among scientists that mammograms did not work as well for women in their 40's, whose denser breasts make tumors harder to spot and who are much less likely than older women to have breast cancer in the first place. To help resolve the question, some urged the cancer institute to halt its promotion of mammograms for these younger women until it did another scientific trial. Instead, in what became a string of flip-flops, the agency in 1977 merely stopped recommending mammograms for women in their 40's. It reversed course in the late 1980's, citing new data that also helped persuade the American Cancer Society and other groups to promote screening for younger women. Then in 1993, still more findings led the institute to abandon the screening recommendation for women in their 40's. Each move was hotly debated, and the issue festered in scientific circles until 1997, when the agency's new director, Dr. Richard Klausner, asked the National Institutes of Health to convene a new panel.
Dr. Leslie R. Laufman, an Ohio cancer specialist, said that before joining the panel, she had never really questioned the evidence about mammograms. At 49, she said, she had been having the screening test herself. "I was walking the walk and talking the talk," she said. But after spending four months reading more than 100 scientific papers and then hearing 32 presentations in a two-day meeting, she and others concluded that women in their 40's should not be told to get screened, and she made a personal decision not have the test herself. The reason was twofold, the panel said. First, the evidence that mammograms helped was tenuous. Second, there were risks in getting screened.
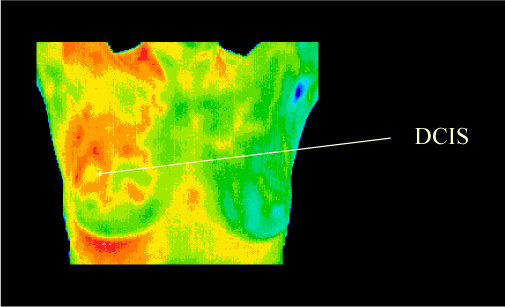
Over the years, scientists have learned that not all breast cancer acts alike. Some tumors grow fast, others slowly. Furthermore, nearly one-fifth of the 230,000 or so cases of breast cancer being found every year are a condition called ductal carcinoma in situ, or D.C.I.S. Mammograms are especially good at finding D.C.I.S. But the problem is that many if not most of these growths — the science on this question is weak — might never spread. Too little is known about breast cancer biology to tell which ones will pose a threat. Thus, women must run the risk of getting unnecessary and dangerous treatment: radiation, chemotherapy, surgery. The panel presented its findings to an audience packed with radiologists and advocates, with boos and hisses punctuating the proceedings. Dr. Klausner created his own stir when he said that he disagreed with the panel.
Then Congress got into the act, instructing the cancer institute to recommend that women in their 40's have mammograms. The institute reversed course and complied. "Now, women in their 40's will have clear guidance based on science and action to match it," President Bill Clinton had said. But if the guidance for women in their 40's was murky, the consensus that screening worked for women in their 50's and 60's would soon be thrown into doubt.
The Doubters of Denmark
Dr. Peter C. Gotzsche said he had never thought much about mammography until the Danish Medical Association asked him to look into it. As director of the Nordic Cochrane Center in Copenhagen, Dr. Gotzsche belonged to a research collective known as the Cochrane Collaboration, which is striving to improve the quality of scientific studies and reporting. When he and his colleague Ole Olsen looked at the seven large clinical trials on mammography, they concluded that they were too flawed to support mammography recommendations, a finding they reported two years ago in the British science journal Lancet. The report drew little public attention. It was their deeper analysis, published in October, that touched off a firestorm.
Dr. Gotzsche and Mr. Olsen cited a number of things they said weakened the research, including potentially inaccurate records of causes of death, differences in screening schedules and possible discrepancies in the health histories of women in one of the trials. In that case, the HIP study in New York, 853 women in the mammography group were excluded because of a previous diagnosis of breast cancer; only 336 were dropped from the unscreened group. If the two groups really were equivalent to start with, and if an extra 500 or so in the unscreened group should have been dropped but were not, that would have been a serious problem, Dr. Gotzsche and Mr. Olsen said. But while some leading medical experts were convinced, many study researchers maintain that the Danish critique misinterpreted data, failed to account for statistical adjustments that corrected problems, read too much into disparities in the numbers and raised alarming questions without offering evidence that the results were actually skewed.
For example, says Dr. Anthony Miller, who reviewed deaths in the HIP trial, the disparity in excluded women would have been a problem only if anyone with a prior history of breast cancer slipped into the final death tallies, thus distorting the results. Systems were put in place to avoid that, he says. "They latched onto these small differences, which have ready explanations, and sort of magnified them," Dr. Miller said. Dr. Gotzsche says he stands by the analysis. "There are no objections that make us doubt what we have done," he said.
The Danish critique also reported that the screened women had more medical and surgical treatments. Treatment is appropriate when it saves lives, but if the death rate from breast cancer was no lower in women who had mammograms, that raises questions, the researchers said, of whether the test does more harm than good. Last month, the panel at the National Cancer Institute concurred with the Danish report and said it would be as rational for a woman to decide not to have the test as to decide to have it. The panel plans to rewrite the assessment that it posts on the cancer institute's Web site.
But others, including scientists who have looked skeptically at mammography over the years, say they are not convinced that the mammography trials were so flawed that their results should be ignored. "Over all, I am not persuaded," said Dr. Suzanne Fletcher of Harvard Medical School, who was chairwoman of a 1993 federal panel that reviewed mammography, "although I thought there were some very important and interesting issues that these authors have raised." Still, Dr. Fletcher and others say they would like to see an independent committee have access to and review the original data from all the trials, including patient records, so that answers might be obtained to the questions the Danish research raised.
A Tool With Limitations
For women and their doctors, the uncertainty is immensely exasperating, given that nearly four decades have passed since researchers began trying to find out if mammograms work. "The bottom line is that if you're still not sure whether it's good or not, it can't be that good," says Dr. Vincent Rajkumar, an oncologist at the Mayo Clinic. "It can't be phenomenally effective." Moreover, scientists say that the value of mammography cannot be weighed without taking into account the complex biology of breast cancer and the increasing effectiveness of treatment. Some tumors grow so fast that mammograms cannot spot them before they spread — and even if they could, the treatment might not be good enough to make any difference. In other cases, the treatment is so effective that it does not matter if the tumor is found with a mammogram or somewhat later, when a lump can be felt, voiding the whole need for early detection.
"An extreme example of that is testicular cancer," says Dr. Peter Greenwald, director of the division of cancer prevention at the National Cancer Institute, "where you can cure all stages, so you don't see a mortality benefit from early detection." For now, even as they acknowledge mammography's limitations, many doctors say it is the best tool they have. While mammograms might not catch some deadly tumors fast enough to make any difference, and they cannot predict which tumors will prove to be deadly, many doctors believe that early detection does help them save some lives.
"I can think of many women where a mammogram was helpful in picking up something before it had spread to the lymph nodes," said Dr. Lynn Hartmann, a breast cancer specialist at the Mayo Clinic. "So I am not at the point of saying we should discard this tool. Until we have a more effective substitute, I continue to recommend mammograms, and I continue to have them." Still, if all the ambiguity is maddening, that is not to say that the debate is unwelcome.
When Dr. Gotzsche took the stage at a conference of the National Breast Cancer Coalition last May to present his work, he checked the path to the exit, fearing he might be run out of the hall. Instead, a third or more of the audience rose to applaud. The group's president, Fran Visco, explained, "Many of our members have long felt that the data is poor, that we oversell screening to the public, that we don't talk about the risks and we don't focus enough attention on preventing breast cancer." "They were thrilled to have someone question all that."